Featured
400 and Counting: UMMC’s Liver Transplant Program Continues to Shine

By Ruth Cummins
UMMC Communications

When Dr. Christopher Anderson performed the University of Mississippi Medical Center’s 389th liver transplant, his focus was on his patient, not what day it was.
March 4, however, was the 10th anniversary of the day in 2013 when UMMC emerged from its 22-year liver transplantation hiatus by giving Jackson resident Karen Battle a life-saving organ. Her surgery began late March 4 and concluded in the wee hours of March 5.
“I’d had a conversation with a couple of people a week or so earlier. Dr. (Mark) Earl said, ‘You realize what’s coming up,’ and I said, ‘Yes, of course, I do,’” remembered Anderson, the James D. Hardy professor and chair of the Department of Surgery and chief of the Division of Transplant and Hepatobiliary Surgery.
“That Monday morning, I woke up and put two and two together, but the day we did the surgery, I didn’t even think about it.”
A decade after Battle’s surgery – she’s healthy and doing well today – the Medical Center performed its 400th liver transplant on May 28. It’s the latest milestone in abdominal transplant at the state’s sole academic medical center.
They include:
- Anderson was recruited in 2011 to jump-start a liver program that had gone by the wayside after faculty and supporting providers dwindled. He built a stellar team for the Division of Abdominal Transplant and Hepatobiliary Surgery, beginning in late 2012 with the hiring of Earl, now professor and surgical director of liver transplantation.
When he accepted the job, Anderson knew access to liver care in his home state was all but non-existent. “But I’m not sure I fully appreciated the degree of it. That hits you in the face when you get here,” he said.
“There were all these patients showing up with late-stage liver disease, late-stage liver cancer, complex liver issues. Their local doctors were doing the best they could do.
“In those first few years, I would describe to colleagues around the country some of these very complex patients that we were seeing and how we handled them, and they said, ‘We’ve never seen this,’ or ‘We’ve only read about that.’ I would say, ‘This is just Monday in Mississippi.’

“Today, we are the only place in the state that offers transplant, and if this program wasn’t here, not only is there no access to liver transplant care, but there’s no access to liver care,” Anderson said.
- Waiting at UMMC for Anderson was Dr. Ashley Seawright, a nurse practitioner recruited in 2007 to help with the kidney transplant program. Her passion would prove invaluable in the revitalization of the abdominal transplant program.
“I helped him build the hepatobiliary program and start the first conference to review cancers in surgical cases,” Seawright said. “From that, we grew the liver program.”
“Ashley is the master of operationalizing things and ideas,” Earl said. “I don’t know if we could have done it without her.”
“I don’t think a single one of us went into this thinking that we were here to be a rock star,” Seawright said. “We did it to provide the services that people need. The patient is the rock star.”
- The abdominal transplant team expanded to include Dr. James Wynn (2014), professor of transplant surgery; Dr. Felicitas Koller (2017), associate professor of transplant surgery; and Dr. Praise Matemavi (2020), assistant professor of transplant surgery.
- The state’s only hepatologist was recruited in 2012 in order to start the program. But a huge boost came in 2020 with the recruitment of Dr. Laura Smart and Dr. Joydeep Chakraborty, both assistant professors in the Division of Digestive Diseases, with Smart leading the hepatology team.
The hiring of Smart and Chakraborty “has been the biggest game-changer for how easily people can access care in our system, and a byproduct of that is more transplants,” Anderson said. “Part of their job is to prevent some patients from progressing to transplant, and delay progression in others.”
- The Medical Center in 2020 recruited its first dedicated transplant infectious diseases team. Dr. Prakhar Vijayvargiya and Dr. Zerelda Esquer Garrigos work with the transplant team to manage the care of that infection-prone population, including patients with HIV.
- The program grew its liver transplant patient coordinators, who include registered nurses Lacey Dungan, Anna McGraw, Taylor Tadlock and Sam Book. Dungan and McGraw hold transplant coordinator certification through the American Board for Transplant Certification.
- Today, abdominal transplant clinics are held in Jackson, Hattiesburg and Grenada, allowing pre- and post-transplant patients to receive a substantial part of their care closer to their home.
“You can’t really talk about the successes of our program without roping in the clinics,” said Dean Henderson, the administrator of transplant services. He was hired in 2013 to provide structure and help grow liver transplant.
“We get attention for the surgery, but it’s those other groups of people who take care of the patients,” Koller said. “It’s an entirely different thing to have a comprehensive liver program, and it’s become much more sophisticated.”
The liver transplant reboot saw 17 more transplants in 2013, growing to 23 in 2014. Last year, it was 50, and so far this year, 24 as of June 21.
The night of Battle’s transplant, she was in the ICU and extremely ill with acute liver and kidney failure, making her very frail and high risk for surgery.
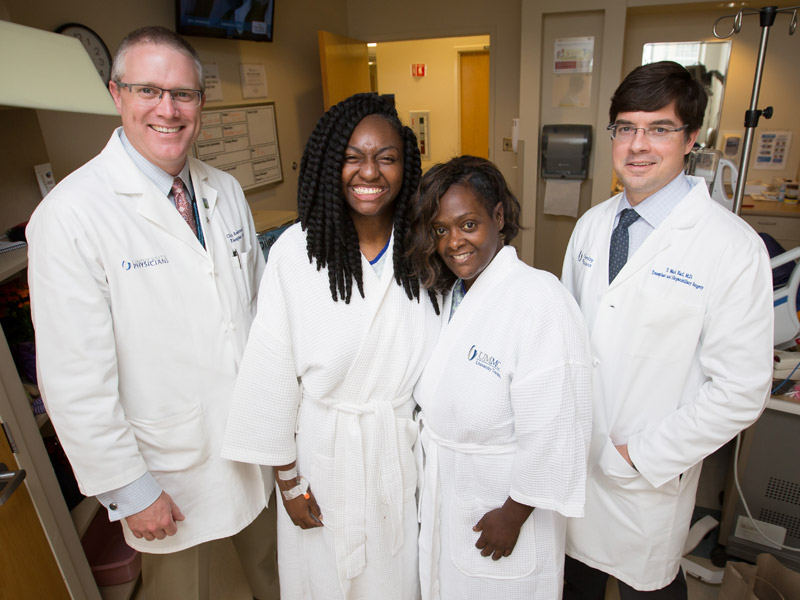
“I vividly remember Dr. Anderson and I standing in the hall in the transplant office, looking at each other,” Earl remembered. “We thought, ‘She is so sick.’ I said, ‘Are we open for business, or are we open for business?’ And he said, ‘Let’s do it.’
“I took off on a plane that evening, brought the donor liver back, and it was a tremendous outcome. It sends chills up my spine.”
More milestones followed, including UMMC’s first liver-kidney transplant in 2014; 100th liver transplant in 2016; first split liver transplant in 2017, in which two women shared a donor liver; first heart-liver transplant in 2018; 200th liver transplant in 2019; and 300th liver transplant in 2021.
One of the early patients was Alenda Carmichael. In the weeks before her September 2014 transplant, she had no idea that her liver was going downhill fast.
A coworker said I didn’t look good, and suggested I go see a doctor,” said Carmichael, a Madison County resident who at the time was a paralegal.
She went to her family doctor, who told her he wanted her to see a gastrointestinal diseases specialist. Carmichael scheduled a morning appointment.
The specialist’s office called her that afternoon. “They said not to panic or rush, but that I needed to go to UMMC now, and they are expecting you. By the time I got to the hospital, my eyes were yellow.”
She went from a regular floor bed to intensive care. “On a Thursday afternoon, the doctors and my liver transplant coordinator told me I was good to go for being on a transplant list,” Carmichael said.
“They had a liver for me in four hours. I had the surgery the next day.”
UMMC’s vast multidisciplinary liver care has been nationally recognized, with the transplant program’s outcomes in 2022 being listed in the top three by the Scientific Registry of Transplant Recipients, a federally controlled organization that compares 148 transplant centers nationwide.
The program received acclaim when Seawright in 2018 was recognized by the American Society of Transplant Surgeons with its Advanced Transplant Provider Award.
The state’s need for liver care is only increasing. “The rates of death in Mississippi from liver disease are not insignificant. The rates of death from liver cancer are not insignificant,” Anderson said. “Having a robust liver transplant program lends itself to an institution having expertise in liver cancer and other complex hepatobiliary cancers.”
To expand UMMC’s program, “we need people. We need physicians. We need staff,” Earl said. “We need more managed care contracts with payors,” meaning more insurance companies making transplant at UMMC in-network for coverage.
More providers and more transplants would at some point require more space on the Medical Center campus. “If this program were to go away, it would be a big public health issue for Mississippi,” Anderson said.
“It’s not just about the surgery. It’s creating an ecosystem that these patients can thrive in,” Koller said. “We are developing a much more comprehensive care model, and we are getting people back to health and well-being.”
Carmichael is grateful for the transplant team who surrounded her then and now. “God made me stronger for the last few months of my husband’s life,” she said of her spouse Mark, who died in 2015.
“I absolutely adore him,” Carmichael said of Earl, her surgeon. “I always said when he entered my room, ‘I must be your favorite person.’ That’s how he treated me.”
“We’ve built over the years an incredible team, from pre-transplant and post-transplant hepatology to pharmacy to nursing to social workers and more,” Earl said.
“I don’t know if we are the best in the country, but I’d sure nominate us.”