Headlines
Ole Miss Alumni Review: New Fertility Test Pioneered At UMMC
Procedure To Gauge Fertility Less Painful, More Accurate
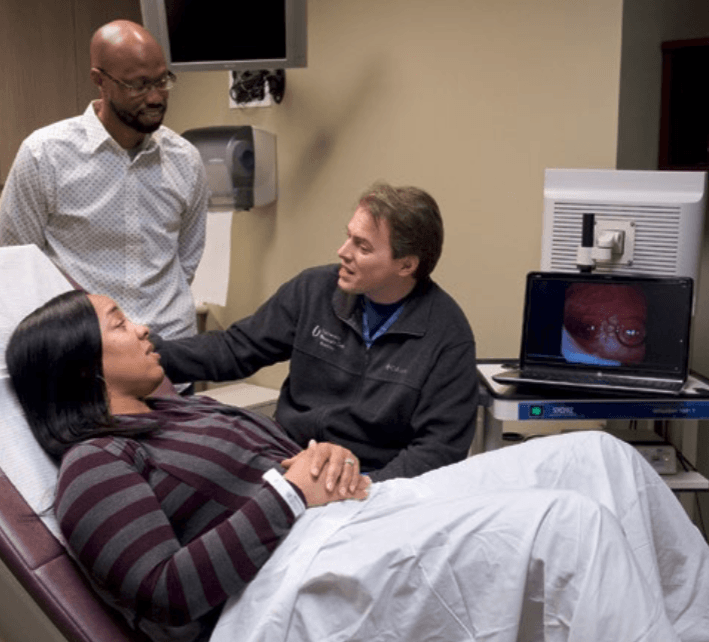
Dr. Preston Parry (right), UMMC associate professor of obstetrics and gynecology, chats with patient Ashley Maryland of Vicksburg. Also pictured is Maryland’s husband, Antonio Maryland. Photo by Jay Ferchaud.
This story was reprinted with permission from the Ole Miss Alumni Review.
Ashley Maryland’s two medical procedures to figure out why she was having trouble becoming pregnant were like night and day.
“It was awful,” Maryland, a Vicksburg resident, says of the hysterosalpingogram, or HSG, performed there in 2013. “It was overwhelming pain, and there was nothing I could do. It was the worst pain ever.”
But her most recent procedure, performed in 2015 by Dr. Preston Parry, University of Mississippi Medical Center associate professor of obstetrics and gynecology, was anything but.
“I anticipated it hurting. I prepared myself for it. But it didn’t hurt at all, and I got to watch it on a screen,” Maryland says.
Not just patients, but their doctors also despise HSG, a test that’s been used for decades to examine a woman’s fallopian tubes to see if they’re blocked. It uses a combination of X-rays and dyes to take a picture of the uterus and typically is done in a hospital. Parry, a reproductive endocrinology specialist and chief of the Division of Reproductive Endocrinology and Infertility, has come up with a technique that minimizes discomfort and is more accurate, faster, cheaper, safer and convenient.
It’s called the Parryscope, which is not a piece of equipment but instead a specific procedure that replaces HSG. During HSG, a physician inserts either a stiff or flexible tube into a woman’s cervix on the way to her uterus. Dye is passed through the inserted tube; if the fallopian tubes are open, the dye will flow through, but if they’re blocked, it won’t.
Patients don’t receive anesthesia, painkillers or drugs to deaden the affected area.
“There are so many women who say it’s the most painful thing they’ve been through,” Parry says. “Women have told me it was worse than childbirth.”
In Parry’s procedure, he uses a narrow, flexible fiber-optic camera, saline and air to determine if the saline and air bubbles can enter the fallopian tubes and if the uterus is receptive to pregnancy. Dye isn’t used at all.
“If the air bubbles don’t go in, the sperm may have trouble getting in, too,” Parry says.
“The camera is the width of a coffee straw,” he says. “We use technology so small and gentle that the speculum for a Pap smear is typically worse.”
To his knowledge, Parry says, no one had previously published data validating the use of a hysteroscope to observe air bubbles and saline for fertility testing. He presented his procedure in October 2015 at a meeting of the American Society for Reproductive Medicine and also at the Open Endoscopy Forum at the Massachusetts Institute of Technology.
“The input was very favorable,” he says of physicians’ reaction to his procedure. “They wanted to know more. The data (show) it’s as accurate, if not more accurate than anything else out there, and light years more gentle.”
An abstract Parry published in September 2015 showed that 88 percent of women undergoing the Parryscope have mild to no discomfort, 10 percent have moderate discomfort, and 2 percent have severe discomfort. His first study of the Parryscope showed that 0.4 percent of women having the Parryscope technique reported extreme discomfort as opposed to 42 percent of those who described that level of pain with HSG.
Risks are associated with both HSG and Parryscope. A woman with a history of gynecologic infections should inform her doctor, who might want to give her antibiotics before the procedure. Vasovagal reactions are rare, and in the case of a Parryscope, it’s possible that air bubbles could travel to the lungs, causing an air embolus.
“Theoretically, this could occur, but in practice and to our knowledge, it has never happened,” Parry says.
Parry says that he continues to research the procedure. Over the past couple of years, he’s done the relatively unknown procedure about 500 times. He says the procedure, although patented, isn’t a moneymaker in itself.
“They may not have the equipment, but I could teach most OB-GYNs how to do this in 10 minutes,” he says.
“The reality is, if you can have a test that’s more accurate, gentler, cheaper and faster, would you do it? Patients overwhelmingly prefer it,” he says. “It’s replacing a test that people passionately hate, and there hasn’t been a viable alternative until now.”
This story was reprinted with permission from the Ole Miss Alumni Review. The Alumni Review is published quarterly for members of the Ole Miss Alumni Association. Join or renew your membership with the Alumni Association today, and don’t miss a single issue.
For questions, email us at hottytoddynews@gmail.com.
Follow HottyToddy.com on Instagram, Twitter and Snapchat @hottytoddynews. Like its Facebook page: If You Love Oxford and Ole Miss…










































