Recent findings that the death rate for cervical cancer is higher than previously reported underline the importance of early detection through screenings similar to those held last month at the Jackson Medical Mall.
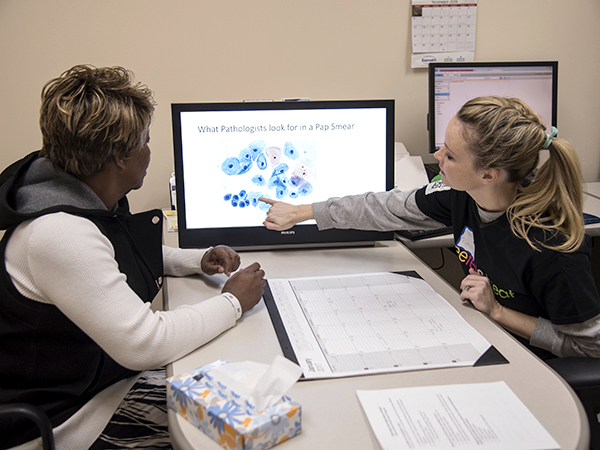
A free cervical cancer screening for women at the University of Mississippi Medical Center came days after authors of a recently published study said the death rate from this preventable cancer is higher than previously reported.
UMMC health care providers joined with community groups to offer free screenings to 41 Jackson metro-area women.
The Jan. 28 screening was part of the College of American Pathologist’s Foundation See, Test & Treat® Program that provides free breast and pelvic cancer screening to underserved women. The screenings, along with one for acral melanoma, were offered by UMMC, CAP and New Horizon Church.
 Dr. Stephen Raab, a UMMC pathologist who has worked with CAP to offer screenings to women who are uninsured or underinsured, said the journal study shows the screening was “even more important. We already have a high death rate, and it may be even higher. It’s important to create screening opportunities and bring patients to this.”
Dr. Stephen Raab, a UMMC pathologist who has worked with CAP to offer screenings to women who are uninsured or underinsured, said the journal study shows the screening was “even more important. We already have a high death rate, and it may be even higher. It’s important to create screening opportunities and bring patients to this.”
Two women who had cervical screenings were referred for diagnostic procedures, and 11 women who had mammograms were referred for diagnostic evaluation.
Cervical cancer is preventable and often can be caught early with a pelvic exam and Pap test that examines cells removed from the cervix. Changes in cervical cells may show up three to seven years before they become cancerous. A Pap test can detect early changes before a malignancy occurs. Removing the cells prevents cervical cancer.
“There are many cancer types that do not have good screening tests. However, the Pap test has been proven to save lives,” said Dr. Kelly Wilkinson, an assistant professor of medicine and a medical oncologist in the gynecologic oncology program.
Researchers writing for Cancer used cancer data from a national program and found black women are dying from cervical cancer at a 77 percent higher rate and white women at a rate 47 percent higher than previously reported.
Researchers from Johns Hopkins Hospital and George Washington University reviewed deaths from cervical cancer for the years 2000-2012. Death rates had been calculated using the number of deaths and the number of women, but the researchers didn’t factor in the number of women who had undergone hysterectomies, including having their cervix removed.
With the new calculations, comparing the deaths to the number of women who had a cervix, the rates rose. So did the racial disparity.
“We’ve always known we had a disparity,” said Deirdre Rogers, director of the Mississippi Cancer Registry, the group that documents cancer incidence in Mississippi. “Black women die of cervical cancer at a much higher rate. They also get it at a much higher rate.
“This is a different way of looking at disparities but it doesn’t alter the fact we’ve always had a disparity,” she said. “The answer is to promote screening and appropriate follow-up after abnormal screenings.”

The researchers found black women had a rate of 10.1 per 100,000 compared to the previous rate of 5.7 per 100,000. For white women, the rate was 4.7 per 100,000 compared to the previous rate of 3.2 per 100,000.
The researchers used data from the National Cancer Institute’s Surveillance, Epidemiology and End Results (SEER) Program for cervical cancer cases and from the Behavioral Risk Factor Surveillance System (BRFSS) for hysterectomy numbers. SEER uses data from 28 states. BRFSS data is based on a telephone survey.
While Mississippi is not included in the SEER database, Rogers said researchers probably would find a similar increase here. The revised numbers reflect a higher rate of deaths, not an increased number of women dying of cervical cancer.
In 2013, the last year for which verified numbers are available, the Mississippi Cancer Registry shows 283 cervical cancer deaths, including 145 black and 134 white women. That same year, the Registry shows 718 women were diagnosed with cervical cancer, including 337 black and 366 white women.
Mississippi ranked 10th nationally in the number of cervical cancer cases diagnosed with 8.1 per 100,000 and first in deaths, 4.0 per 100,000, according to the U.S. Cancer Statistics Working Group.
 “Our disparities focus in areas that are underserved,” said Dr. Mildred Ridgway, assistant professor of obstetrics and gynecology and a gynecologic oncologist in the gynecologic oncology program. “Access to care and education are the number 1 and 2 things we need to do to change this.”
“Our disparities focus in areas that are underserved,” said Dr. Mildred Ridgway, assistant professor of obstetrics and gynecology and a gynecologic oncologist in the gynecologic oncology program. “Access to care and education are the number 1 and 2 things we need to do to change this.”
Some women in rural areas have limited access to medical care and screening. Social disparities in more urban areas may prevent some women from getting appropriate screening, she said.
At UMMC, she sees more black women with later-stage cervical cancer, equating to a higher mortality, a finding reflected in the recent research paper.
“Cervical cancer can be a life-threatening disease. However, with appropriate early intervention, it is easily preventable and treatable,” said Wilkinson.
Ridgway and Wilkinson encourage human papillomavirus vaccinations. HPV is a significant factor in more than 90 percent of cervical cancer cases. The virus may clear on its own, but if it doesn’t, it becomes a risk factor in several cancers.
Vaccinations are recommended for girls and boys ages 9-26. Cervical cancer screening is recommended for women ages 21-65.
“Vaccination against this virus can help prevent the development of cervical cancer,” Wilkinson said.
Together, regularly recommended screening and vaccination would significantly lower the cases and deaths. Doctors hope that FOX Sports NFL sideline reporter Erin Andrews’ announcement that she has successfully battled cervical cancer will encourage more women to be screened. Hers was caught in a routine health exam and cleared with surgery.
For questions or comments, email hottytoddynews@gmail.com.
